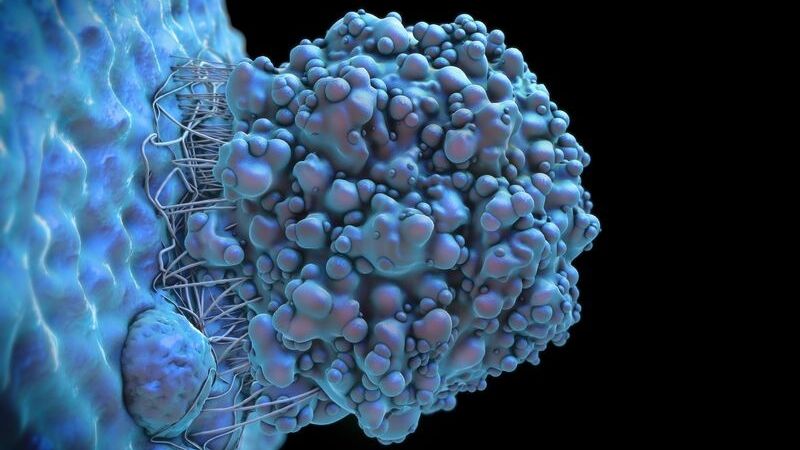
Credit: iStock
Johns Hopkins researchers report that a type of biodegradable, lab-engineered nanoparticle they fashioned can successfully deliver a “suicide gene” to pediatric brain tumor cells implanted in the brains of mice. The poly(beta-amino ester) nanoparticles, known as PBAEs, were part of a treatment that also used a drug to kill the cells and prolong the test animals’ survival.
In their study, described in a report published January 2020 in the journal Nanomedicine: Nanotechnology, Biology and Medicine, the researchers caution that for safety and biological reasons, it is unlikely that the suicide gene herpes simplex virus type I thymidine kinase (HSVtk) — which makes tumor cells more sensitive to the lethal effects of the anti-viral drug ganciclovir — could be the exact therapy used to treat human medulloblastoma and atypical teratoid/rhabdoid tumors (AT/RT) in children.
So-called “suicide genes” have been studied and used in cancer treatments for more than 25 years. The HSVtk gene makes an enzyme that helps restore the function of natural tumor suppression.
Specifically, the experiments found that a combination of the suicide gene and ganciclovir delivered by intraperitoneal injection to mice killed more than 65% of the two types of pediatric brain tumor cells. The combination was deliberately “transfected” with the gene seven days after the nanoparticle therapy was used to deliver the genetic material. Mice bearing an AT/RT-type tumor lived 20% longer after receiving the treatment — 42 days, compared to 35 days for untreated mice. Those with a group 3 medulloblastoma-type tumor implanted in the brain lived 63% longer, surviving 31 days compared to 19 days for untreated mice.
“It’s an exciting alternate way to be able to deliver gene therapy to a tumor in a selective fashion that targets only tumor cells,” says Eric Jackson, M.D., associate professor of neurosurgery at the Johns Hopkins University School of Medicine. “Our idea now is to find other collaborators who may have a gene therapy that they think would work well to kill these tumors.”
Medulloblastoma and AT/RT are two of the most prevalent and deadly pediatric brain malignancies. Traditional treatments, including radiation, can harm healthy tissue as well as the tumor, and can produce long-lasting developmental side effects in growing children, making it critical to find new therapies, Jackson notes.
Gene therapy that targets only cancer cells is a promising treatment avenue, but many gene therapy methods use a modified virus to deliver their therapeutic payloads of DNA, a method that may not be safe or suitable for pediatric use. “A lot of these viruses are safe if you have a mature immune system, but in very young patients with more fragile immune systems, a virus delivery system may pose additional risks,” says Jackson.
To address this issue, Jackson collaborated with Jordan Green, Ph.D., an investigator at the Johns Hopkins Kimmel Cancer Center Bloomberg~Kimmel Institute for Cancer Immunotherapy, director of the Johns Hopkins Biomaterials and Drug Delivery Laboratory and professor of biomedical engineering, to find a different kind of carrier for gene therapy. Green and his colleagues developed the PBAE class of polymeric nanoparticles, which can be engineered to bind and carry DNA.
The biodegradable PBAEs are injected into a tumor mass where they safely release their DNA cargo after being ingested by tumor cells. In previous studies that used similar particles to deliver gene therapy to adult brain cancers and liver cancers in cell cultures and in rodents, Green and his colleagues found that the nanoparticles preferentially target tumor cells over healthy cells.
The mechanism that allows the particles to target tumor cells preferentially is still being investigated, but Green thinks “the chemical surface of the particle is likely interacting with proteins that are on the surface of certain types of cancer cells.”
Green and his colleagues altered the nanoparticles to target the two pediatric malignancies. “By making small chemical changes to the polymers that make up the nanoparticles, we can significantly change the cellular uptake into particular kinds of cancer cells, and the subsequent gene delivery to the cytosol, in a cell-specific way,” Green says.
Jackson says he hopes the nanoparticles can be used to deliver a variety of gene-based treatments – including therapies that alter the expression levels of genes, turn genes on and off altogether, or sensitize cells to other therapies – depending on the specifics of a patient’s tumor. “In some ways, we’re still in the discovery phase of what genes to target” in medulloblastoma and AT/RT, he says.
The nanoparticles “can carry larger genes than what can be carried by a virus, and can carry combinations of genes,” says Green. “It’s a platform that doesn’t have limitations on the cargo size being delivered, or limitations related to immunogenicity or toxicity. And, it is easier to manufacture than a virus.”
Other Johns Hopkins researchers involved in the study were John Choi, Yuan Rui, Jayoung Kim, Noah Gorelick, David Wilson, Kristen Kozielski, Antonella Mangraviti, Eric Sankey, Henry Brem and Betty Tyler.
The research was supported by the National Institutes of Health (R01CA228133).
The scientists are filing for patents related to this work.