In a new study on mice, Johns Hopkins Medicine researchers report that using MRI scans to measure blood volume in the brain can serve as a noninvasive way to potentially track the progress of gene editing therapies for early-stage Huntington’s disease, a neurodegenerative disorder that attacks brain cells. The researchers say that by identifying and treating the mutation known to cause Huntington’s disease with this type of gene therapy, before a patient starts showing symptoms, it may slow progression of the disease.
The findings of the study were published May 27 in the journal Brain.
“What’s exciting about this study is the opportunity to identify a reliable biomarker that can track the potential success of genetic therapies before patients start manifesting symptoms,” says Wenzhen Duan, M.D., Ph.D., director of the translational neurobiology laboratory and professor of psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine. “Such a biomarker could facilitate the development of new treatments, and help us determine the best time to begin them.”
Huntington’s disease is a rare genetic disorder caused by a single defective gene, dubbed “huntingtin,” on human chromosome 4. The gene is passed on from parents to children — if one parent has the mutation, each child has a 50% chance of inheriting it. Huntington’s disease has no cure and can lead to emotional disturbances, loss of intellectual abilities and uncontrolled movements. Thanks to genetic testing, people can know if they have the disease long before symptoms arise, which typically happens in their 40s or 50s.
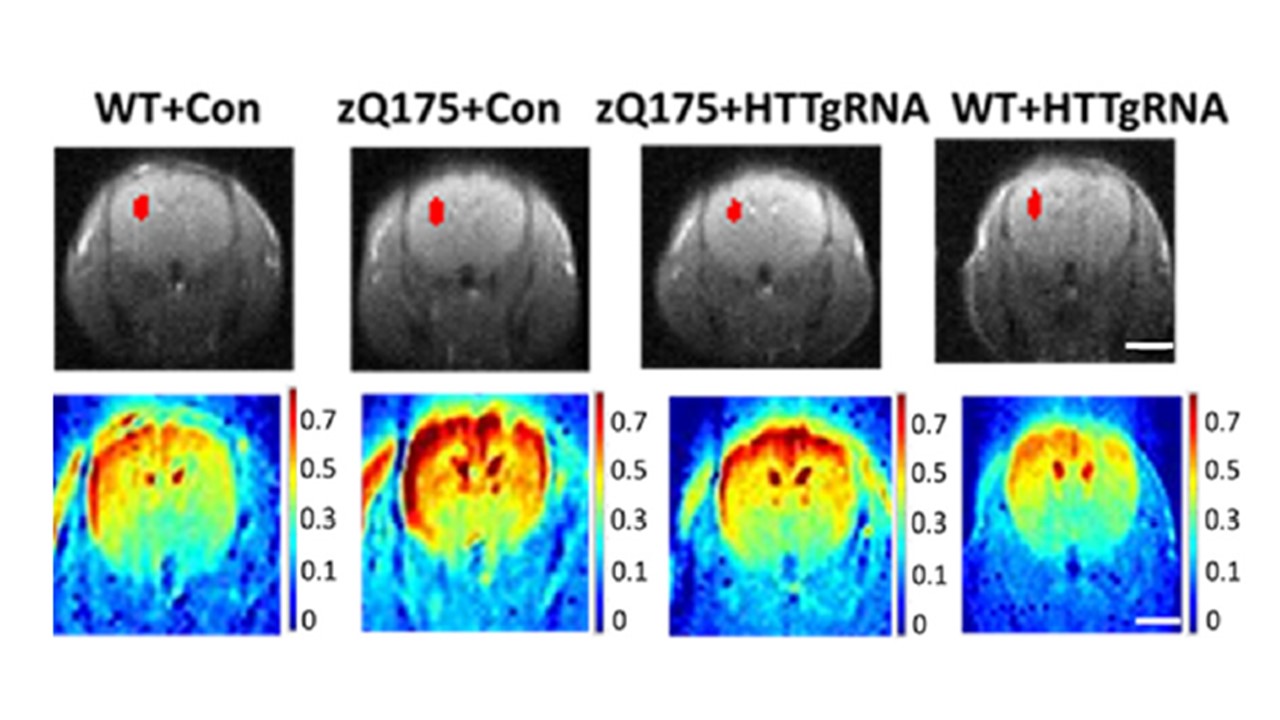
For the study, Duan and her team collaborated with colleagues from Kennedy Krieger Institute in Baltimore, Maryland, who developed a novel method to more precisely measure the blood volume in the brain by using advanced functional MRI scans. With the scans, they can map the trajectory of blood flow in small blood vessels called arterioles in the brains of mice engineered to carry the human huntingtin gene mutation that mirror the early stages of Huntington’s disease in humans.
Duan notes that there are many known metabolic changes in the brains of people with Huntington’s disease, and those changes initiate a brain blood volume response in the disease’s early stages. Blood volume is a key marker for oxygen supply to brain cells, which in turn supplies energy for the neurons to function. But with Huntington’s disease, the brain’s arteriolar blood volume is dramatically diminished, which makes the neurons deteriorate because of lack of oxygen as the disease progresses.
In a series of experiments, the researchers suppressed the mutation in the huntingtin gene in mice, using a gene-editing technology known as CRISPR — a tool for editing genomes that allows the alteration of a DNA sequence to modify gene function. Then, they used the MRI scanning technique and other tests to track the brain function over time both of mice with the huntingtin mutation, in which they edited out the faulty gene sequence, and a control group of mice in which the faulty gene was unedited.
The experiments assessed abnormalities in the trajectory of arteriolar blood volumes in mouse brains with the Huntington’s disease mutation at 3, 6 and 9 months of age (pre-symptom stage, beginning of symptoms and post-symptom stage, respectively). The researchers looked at whether suppression of the mutant huntingtin gene in the neurons could normalize altered arteriolar blood volumes in the pre-symptom stage, and whether reduced expression of the huntingtin gene at the pre-symptom stage could delay or even prevent development of symptoms.
“Overall, our data suggest that the cerebral arteriolar blood volume measure may be a promising noninvasive biomarker for testing new therapies in patients with Huntington’s who are yet to show symptoms of the disease,” says Duan. “Introducing treatment in this early stage may have long-lasting benefits.”
When the researchers mapped the trajectory of cerebral blood volume and conducted an assortment of brain and motor tests in the mice at 3 months of age, and compared the test to those of the control group, they observed no significant differences except in cerebral blood volumes. However, Huntington’s symptoms in the mice with the huntingtin gene started at 6 months of age and progressively worsened at 9 months, suggesting that altered cerebral blood volume occurs before motor symptoms and atrophy of the brain cells — typical traits of the disease.
The cerebral blood volume changes were also found to be similar to those observed in patients with Huntington’s disease before they start manifesting symptoms, which declines with the start of symptoms and while the disease progresses over time.
The researchers also analyzed the structure of the arteriole blood vessels in the brains of mice with the mutant huntingtin gene at 3 and at 9 months of age and found no differences in the numbers of vessel segments in the pre-symptom stage. However, they observed that smaller blood vessels had an increased density and reduced diameter, which may be a vascular response to compensate for the impaired neuronal brain function. This might suggest, the researchers conclude, that impaired vascular structure leads to lowered arteriole blood volumes and possibly compromised ability to compensate for the loss in the symptom stage.
Considering that Huntington’s disease symptoms depend not only on brain cell loss but also on how neurons deteriorate, the researchers set out to determine if suppressing the huntingtin gene during the pre-symptom stage in mice could delay or even prevent disease progression. To do that, the researchers introduced the altered huntingtin gene to the neurons in mice at 2 months of age and evaluated the outcomes at 3 months of age (when no atrophy or motor deficits were present).
Remarkably, the researchers say, the cerebral arteriolar blood volume in mice with the altered huntingtin gene was This suggests that the altered cerebral blood volume during the pre-symptom stage in mice is most likely due to neuronal changes in either activity or metabolism.
“Our findings demonstrate that significant changes in arteriolar cerebral blood volumes occur before neurons start to degenerate and symptoms begin, further supporting the idea that altered cerebrovascular function is an early stage symptom in Huntington’s disease,” says Duan. She explains that these changes also indicate there’s a pre-symptom therapeutic window in which to test interventions. While no animal model replicates all the symptoms of human Huntington’s disease, this research offers an alternative system to study functional changes in the pre-symptom stage, she says.
Further validation of these findings in human clinical trials would facilitate development of efficient therapeutic interventions for patients with Huntington’s disease before they start developing symptoms. “The goal is to delay or even conceivably prevent the manifestation of Huntington’s disease altogether,” says Duan.
Along with Duan, other researchers who contributed to the work are Hongshuai Liu, Chuangchuang Zhang, Jing Jin, Liam Cheng, Qian Wu, Zhiliang Wei, Peiying Liu and Christopher Ross from Johns Hopkins, and Jiadi Xu, Xinyuan Miao, Hanzhang Lu, Peter van Zijl and Jun Hua from the Kennedy Krieger Institute and Johns Hopkins.
