Drug “hides” insulin-producing beta cells in mice
Scientists at Johns Hopkins Medicine say that an experimental monoclonal antibody drug called mAb43 appears to prevent and reverse the onset of clinical type 1 diabetes in mice, and in some cases, to lengthen the animals’ lifespan.
The drug is unique, according to the researchers, because it targets insulin-making beta cells in the pancreas directly and is designed to shield those cells from attacks by the body’s own immune system cells. The drug’s specificity for such cells may enable long-term use in humans with few side effects, say the researchers. Monoclonal antibodies are made by cloning, or making identical replicas of, an animal (including human) cell line.
The findings, reported online recently and in the May issue of Diabetes, raise the possibility of a new drug for type 1 diabetes, an autoimmune condition that affects about 2 million American children and adults and has no cure or means of prevention. Unlike type 2 diabetes, in which the pancreas makes too little insulin, in type 1 diabetes, the pancreas makes no insulin because the immune system attacks the pancreatic cells that make it.
The lack of insulin interferes with the body’s ability to regulate blood sugar levels.
“People with type 1 diabetes face lifelong injections of insulin and many complications, including stroke and eyesight problems if the condition is not managed properly,” says Dax Fu, Ph.D., associate professor of physiology at the Johns Hopkins University School of Medicine and leader of the research team.
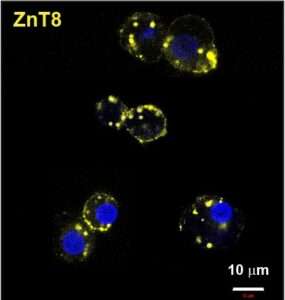
Fu says mAb43 binds to a small protein on the surface of beta cells, which dwell in clusters called islets. The drug was designed to provide a kind of shield or cloak to hide beta cells from immune system cells that attack them as “invaders.” The researchers used a mouse version of the monoclonal antibody, and will need to develop a humanized version for studies in people.
For the current study, the researchers gave 64 non-obese mice bred to develop type 1 diabetes a weekly dose of mAb43 via intravenous injection when they were 10 weeks old. After 35 weeks, all mice were non-diabetic. One of the mice developed diabetes for a period of time, but it recovered at 35 weeks, and that mouse had early signs of diabetes before the antibody was administered.
In five of the same type of diabetes-prone mice, the researchers held off giving weekly mAb43 doses until they were 14 weeks old, and then continued dosages and monitoring for up to 75 weeks. One of the five in the group developed diabetes, but no adverse events were found, say the researchers.
In the experiments in which mAb43 was given early on, the mice lived for the duration of the monitoring period of 75 weeks, compared with the control group of mice that did not receive the drug and lived about 18–40 weeks.
Next, the researchers, including postdoctoral fellows Devi Kasinathan and Zheng Guo, looked more closely at the mice that received mAb43 and used a biological marker called Ki67 to see if beta cells were multiplying in the pancreas. They said, after treatment with the antibody, immune cells retreated from beta cells, reducing the amount of inflammation in the area. In addition, beta cells slowly began reproducing.
“mAb43 in combination with insulin therapy may have the potential to gradually reduce insulin use while beta cells regenerate, ultimately eliminating the need to use insulin supplementation for glycemic control,” says Kasinathan.
The research team found that mAb43 specifically bound to beta cells, which make up about 1% or 2% of pancreas cells.
Another monoclonal antibody drug, teplizumab, was approved by the U.S. Food and Drug Administration in 2022. Teplizumab binds to T cells, making them less harmful to insulin-producing beta cells. The drug has been shown to delay the onset of clinical (stage 3) type 1 diabetes by about two years, giving young children who get the disease time to mature and learn to manage lifelong insulin injections and dietary restrictions.
“It’s possible that mAb43 could be used for longer than teplizumab and delay diabetes onset for a much longer time, potentially for as long as it’s administered,” says Fu.
“In an ongoing effort, we aim to develop a humanized version of the antibody and conduct clinical trials to test its ability to prevent type 1 diabetes, and to learn whether it has any off-target side effects,” says Guo.
Other scientists who contributed to the research include Dylan Sarver, G. William Wong and Maria Golson from Johns Hopkins; Shumei Yun from the University of Maryland, Aaron Michels and Liping Yu from the University of Colorado; and Chandan Sona and Matthew Poy from Johns Hopkins All Children’s Hospital.
Funding for the research was provided, in part, by the National Institutes of Health (R01DK125746, P30DK116073, R01DK110183, R01 DK135688 and RO1DK084171).
DOI: doi.org/10.2337/db23-0568
Media Contacts
Vanessa Wasta
