KL2 Clinical Research Scholar Amir Manbachi, MSc, PhD co-leads the team in developing the technology discussed in the article below.
From the moment a patient arrives at The Johns Hopkins Hospital with a spinal cord injury that is treatable by surgery, clinicians prepare for spinal decompression and a procedure for stabilization. But after an operation is performed, “we can’t monitor the spinal cord and provide treatment interventions in real time,” says Nicholas Theodore, MD, MS, director of the Johns Hopkins Neurosurgical Spine Center. That all may change, however, thanks to a $13.48 million grant from the Defense Advanced Research Projects Agency and a team of Johns Hopkins neurosurgeons and biomedical engineers, working in tandem with academic and industry partners.
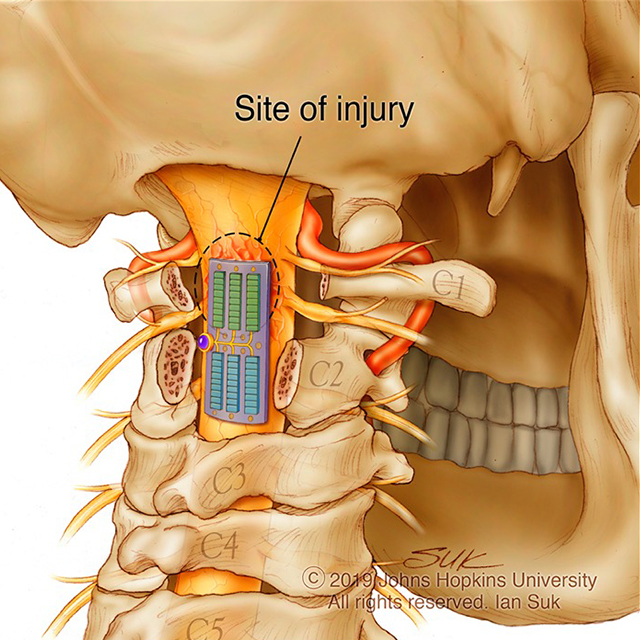
The group — led by Theodore and biomedical engineer Amir Manbachi, MSc, PhD — is developing both implantable and wearable devices to be implemented at the time of surgery to allow continuous, postoperative treatment of acute, subacute and chronic spinal cord injury. The technologies’ shared purpose is to prevent secondary injury such as neurological damage, hypoxia, neurogenic shock, hemorrhage, edema and glial scarring, and to promote immunomodulation and neuromodulation for lower extremity muscle function, cardiovascular stability and bladder function.
The team’s goal is to build and test three implantable devices and three wireless wearables that would work together to monitor perfusion pressure, oxygenation, intrathecal pressure, temperature and other biomarkers, as well as deliver interventions.
“If we could measure, monitor and treat the perfusion pressure of the spinal cord continuously over the course of a week or more after surgery, it would give us a real opportunity to improve outcomes,” says Theodore.
The technology includes a multifunctional implant that would be placed epidurally at the site of the injury to perform ultrasound imaging, focused ultrasound, biomarker sensing and electrical spinal stimulation; an epidural electrical spinal stimulator; and an acute CSF management implant in the subarachnoid space that would monitor intrathecal pressure, oxygenation and temperature of CSF. Communication between the CSF management implant and the multifunctional implant would allow precise drainage of CSF and restoration of autoregulation.
The wireless wearables include a blood pressure imaging sensor, a bladder volume imaging and pressure sensor, and an electromyography and accelerometry tracking sensor. These technologies would deliver real-time data to one software application that will help inform treatment decisions.
Today, there is no way to consistently monitor opportunities for promising interventions such as CSF drainage and maintenance of mean arterial pressure, says Theodore. Likewise, he believes electrophysiological and ultrasound stimulation may hold promise for patients, and one of his first priorities is testing how pulsed ultrasound affects blood flow and exploring ways it can be used therapeutically as well as diagnostically.
The team aims to have an FDA-approved technology that could be used in clinical trials by the end of the five-year grant period.
“We have the top neurosurgery department in the country combined with the top biomedical engineering department in the country on this project,” says Theodore. “I’m extremely optimistic about the possibilities.”
By Lisa Eddy
PUBLISHED IN NEUROLOGIC WINTER 2021
