A national, multicenter clinical trial (BMT CTN 1507) of low-dose haploidentical (half-matched) bone marrow transplant to treat severe sickle cell disease found the treatment to be safe and curative for adults with serious sickle cell-related health complications.
The findings from the phase II clinical trial will be featured Dec. 12 as a high-impact study (abstract #LBA4) at the annual meeting of the American Society of Hematology (ASH).
“Our findings show that matched donors — available to only a few of the patients with sickle cell disease — are no longer required for cure of the disease with allogeneic transplantation,” says Robert Brodsky, M.D., director of hematology at the Johns Hopkins University School of Medicine and study co-leader. “Reduced-intensity haploidentical bone marrow transplant is a safe, curative therapy suitable for adults with sickle cell disease who also have complications related to their disease, such as organ damage, stroke or pulmonary hypertension, making it a treatment option for many more patients.”
The clinical trial included 42 individuals with sickle cell disease. Most participants were African American (92.6%), and the median age was 22. Of the 42 participants, 95% were still alive two years after transplant, and 88% have not seen their sickle cell disease return and are considered cured.
“These data confirm results from Johns Hopkins and Vanderbilt, where longer follow-up demonstrates that virtually all patients beyond two years from transplant without disease are cured,” says Brodsky.
Patients in the clinical trial — sponsored by the National, Heart, Lung, and Blood Institute and the National Cancer Institute — were treated with a reduced-intensity (low dose) haploidentical bone marrow transplant at 19 hospitals across the U.S. In this type of bone marrow transplant, the donated bone marrow comes from a half-matched donor, such as a patient’s parent, sibling or child. Other relatives, including a nephew, niece, aunt or uncle, are also often suitable donors. Patients were treated with low-dose therapy to prepare them for transplant, and were given post-transplant cyclophosphamide, a drug that earlier research has proven to stave off graft-versus-host disease, a complication in which the immune cells in the donor marrow attack their new host, the patient.
Haploidentical bone marrow transplant with post-transplant cyclophosphamide was developed through more than a half-century of translational team science at the Johns Hopkins Kimmel Cancer Center. This study included small modifications made by the Vanderbilt research team.
A high-dose regimen, known as myeloablative conditioning, with a fully matched bone marrow transplant has been known to cure sickle cell disease for decades. However, its use has been limited — particularly in older patients with organ damage caused by sickle cell disease — because of concerns about side effects, says Brodsky. Such patients are also often excluded from myeloablative gene therapy and gene editing trials, he adds.
In the reduced intensity, haploidentical transplant study, serious side effects were uncommon. They included one graft failure; moderate to severe graft-versus-host disease (26.2%) and two deaths in the first year post-transplant.
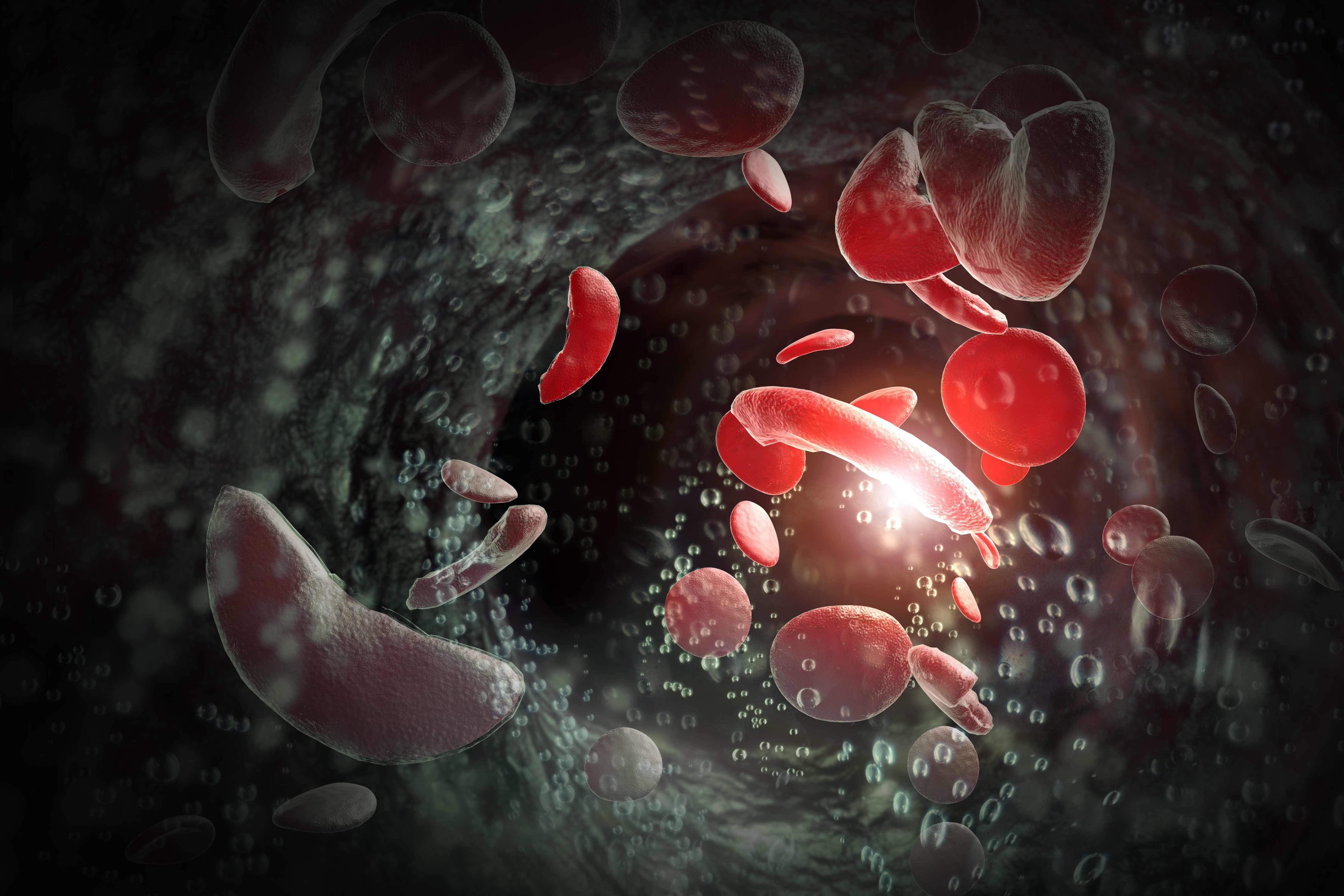
Sickle cell disease affects about 100,000 Americans, primarily African Americans, and 20 million people worldwide. It is a painful, blood disorder in which red blood cells are shaped like crescents instead of discs, and clog up blood vessels.
In addition to Brodsky, other study co-leaders were Michael DeBaun, M.D., director of the Vanderbilt-Meharry Center for Excellence in Sickle Cell Disease, Adetola Kassim, M.D., M.S., director of the Adult Sickle Cell Disease Program at the Vanderbilt-Ingram Cancer Center, and Mark Walters, M.D., division chief of hematology at the UCSF Benioff Children’s Hospitals.
The research was funded by the National Heart, Lung, and Blood Institute (U10HL069294) and the National Cancer Institute (U24HL138660).
Media Contacts
Amy Mone
[email protected]
Valerie Mehl
[email protected]
